NCSA interview with an autism mom about her daughter’s experience with transcranial magnetic stimulation
Background
In February 2019, NCSA published a blogpost called, "Autism: Miswiring and Misfiring in the Cerebral Cortex," by Manuel Casanova, MD. He explained the evidence that autism can be rooted in pathologies of brain development, specifically abnormal micro-structural development of the “minicolumns” of the cerebral cortex, and further that this physiological defect had potential implications for therapeutics.
Dr. Casanova discussed that the cerebral cortex is the part of the brain that enables us to process sensory information, engage in complex thought and abstract reasoning, and produce and understand language. It accounts for our volitional actions including those that allow us to adapt to our immediate environment. But in autism we see the failure of connections — cells in the cerebral cortex are not able to coordinate their actions with other cells in their surroundings.
He then explained that these findings may suggest a therapeutic intervention based on transcranial magnetic stimulation (TMS). TMS works on the principle of induction of electricity. A strong magnetic field induces current through anatomical elements in the cerebral cortex that act as conductor. Due to the geometrical orientation of anatomical elements within the periphery of the cortical minicolumns, inhibitory elements are stimulated when using low frequency stimulation. This intervention allows us to rebuild the “shower curtain” surrounding the minicolumns.
He said that several hundred high functioning ASD patients have been treated with TMS with positive results, primarily in terms of improving executive functions and reducing perseveration.
This interview with autism mom Jan Kasahara is something of a follow-up to Dr. Casanova’s article. It is not meant to offer medical advice, and does not constitute an endorsement of this intervention. Rather, the purpose of this interview is to highlight the extremely urgent need for therapeutics for severe autism, and that this therapy may warrant greater scientific attention for low-functioning individuals.
Interview
NCSA: Jan, we wanted to give our community a chance to hear about your experience, because you have a daughter who has who is severely impacted by autism and who underwent this experimental treatment, which is very unusual. Please give us a bit of background about Madison.
JK: Madison is 22. We adopted her from China as a baby, and at the age of three she received a diagnosis of autism. She started talking and then stopped. She started hand flapping, spinning in circles, not wearing clothes, climbing on everything — pretty much showing many signs of low functioning autism. And since then, it's been a struggle to try and find something to help her.
She has severe OCD. She will hit her chin if she can't put all of her movies away. She will get upset in the car if we don’t go a certain direction. She would be constantly upset, often screaming, having trouble trying to show me what she wants. She can't point. She has trouble with tags on her clothes, she'll only wear crocs and won’t wear regular shoes. Very little eye contact and she can't really do anything functional, for example she can't brush her hair, she can't dress herself, she cannot help with anything around the house. She basically would sit on the couch and do YouTube all day or movies.
NCSA: Obviously one can see why a parent in your situation would be very eager to find something that could help her.
JK: I think the number one problem with her is language. I was really hoping to find something to help her achieve some form of language because I think that is a lot of her frustration. Also, she has a huge amount of anxiety, which was very, very high. She seemed like she'd always struggle with that or depression. She had no initiation. She didn't really care about people or what she was they were doing, so her quality of life was just so low. And I was just trying to think of anything that would help her quality of life.
NCSA: So what how did you come across the idea to try TMS?
JK: To be honest, I was on YouTube, and like any autism mom, trying to find anything that I could possibly find. And I fell upon a clinic based in San Mateo, which is not far from our home in the Bay Area. And there was also a little blurb about it from the TV show The Doctors about a young girl who had autism, and TMS helped her start speaking.
I am definitely one of those moms who is unafraid to experiment. So I researched it and spoke with the clinic’s director. So I met up with him and I felt really comfortable with him.
NCSA: To be clear, this treatment was not covered by insurance, just a private pay enterprise on your part.
JK: Our claim was denied but we are resubmitting it with more information. The six-week treatment was more than 10,000 dollars.
NCSA: Please tell us what the therapy consisted of, and any difficulties experienced by Madison.
Well, first they need to do an EEG to look at her brainwaves to see more precisely what is going on. I’m hardly a neuroscientist but I’ve learned that with a lot of kids with autism, they find that their brain waves aren't functioning completely, which is associated with depression, anxiety, and insomnia. The waves are very flat.
In the EEG she had to wear a tight cap on her head with little electrodes. So we practiced at home, putting a bathing cap, shower cap and knitted beanie, anything to try and get her used to have something on her head. But once we got her in there, they were so sweet and they really made it easy for her. They need 10 minutes of quality data with her eyes closed, motionless and quiet. With Madison, the process took from 10 minutes to 40 minutes depending on how calm she was that day.
The EEG showed that basically her brain waves were pretty flat. He could tell also by looking at the brain waves that she wasn't sleeping, had a lot of depression and anxiety. The clinic had not worked with a lot of kids on the spectrum this severe, and they couldn’t promise anything regarding the treatment, but I decided to just go ahead. It was worth a try.
They developed a treatment plan based on the EEG, such as where they put the magnet, how strong they want to make it. In her case, they put it in the front part of the cortex and behind in the back of her head. The magnet is like a heavy, flat wand, with a handle and makes a clicking sound as they put it against the head to stimulate the brain.
It was of course challenging to keep Madison sitting still. I'm not going to say it was easy. She did get upset. The doctor actually made sure that he brought in Oreos, her favorite, to entice her to stay in the seat, which is like a leather recliner chair. They also have a weighted blanket and toys and would play movies and music videos. Some of the kids end up running down the halls and they just go retrieve them and bring them back and they really try their best.
NCSA: So how long did Madison have to sit in the chair for each session?
JK: About 30 minutes.
NCSA: Yeah, that would be hard for a lot of our kids. How many sessions did she do?
JK: So 30 minutes, five days a week for two weeks — that was the first set of sessions, and then we did two more sets. About 30 treatments altogether.
NCSA: But as you said, you’re a mom who is willing to try almost anything, you’re taking one for the team. So did you notice any changes in Madison right off the bat?
JK: It seemed like her anxiety did go down. I noticed that she was a lot calmer and she seemed more affectionate, which was something different. She was actually cuddling with me on the couch, which she had not really done before, and she was looking into my eyes more. She didn't seem as fearful like she was. So those were the main things in the very beginning. A lot of the fear, a lot of the depression and anxiety had seemed to go down and she seemed to be more affectionate.
NCSA: Then after the three sets of treatments?
The treatments ended in March and now we’re in June. I noticed her speech started getting a little bit clearer, including some new words. One night we were in her bedroom and I would hold up a book and she said “book.” And then I would hold something else like a bear, and she'd say, “bear.” It was so exciting, and she was just so fun. She was so happy.
She seemed to have more initiative. She had gone into the bathroom and I noticed that she'd taken the toothpaste and put it on her toothbrush, something she had never done, and she started brushing her teeth back and forth. So even her motor planning got better. Before she would just bite her toothbrush, but I actually saw her brushing back and forth. Then she'd take a hairbrush out and she'd start brushing her hair. That was just too much. That was something she would never do. So I could see that there was a lot of initiative happening. And that was very exciting.
I took her to the store yesterday and I thought to myself, she's not rocking back and forth on her feet like she normally does. She’s normally stimming with her hands, making all kinds of echolalia, walking into people. And she was just standing there, calm. It was so strange.
Recently she got all the dolls out of the garage. She had never played with dolls before. She brought them into the family room and she started pretend play. She started brushing their hair and changing their clothes and went and got the bed and put them in the bed - without anybody prompting her.
At school, they've told me they can't believe how great she's doing. She's not running into other classrooms like she always did. She's staying in the classroom. She's actually helping wash the dishes, which she's never done. She can ride the bike. She used to scream for somebody to help her get on the bike, but now she just gets on the bike by herself and goes. She doesn't scream anymore.
NCSA: The reason we wanted to publish something about your experience is not to make any claims about the treatment (this is classic n=1) but to stress that for kids like ours the need for progress is so urgent — we desperately need to find interventions that can increase functional capacity, improve quality of life, alleviate terrible symptoms. We need a more intensive research effort to find valid interventions.
JK: Absolutely! Our kids are suffering every day. They are behind a wall where they can't even express for themselves what's going on. They're depressed. They are dealing with trying to move their bodies and their bodies won't do what they want to do. They're hitting themselves. They're impulsive. These are kids who are going to need immense amount of help in the future. And if we can't find help for our kids, they're going to have a terrible life. They're going to suffer, and the last thing we want for our children. More and more kids have an autism diagnosis. The need to help them is absolutely desperate.
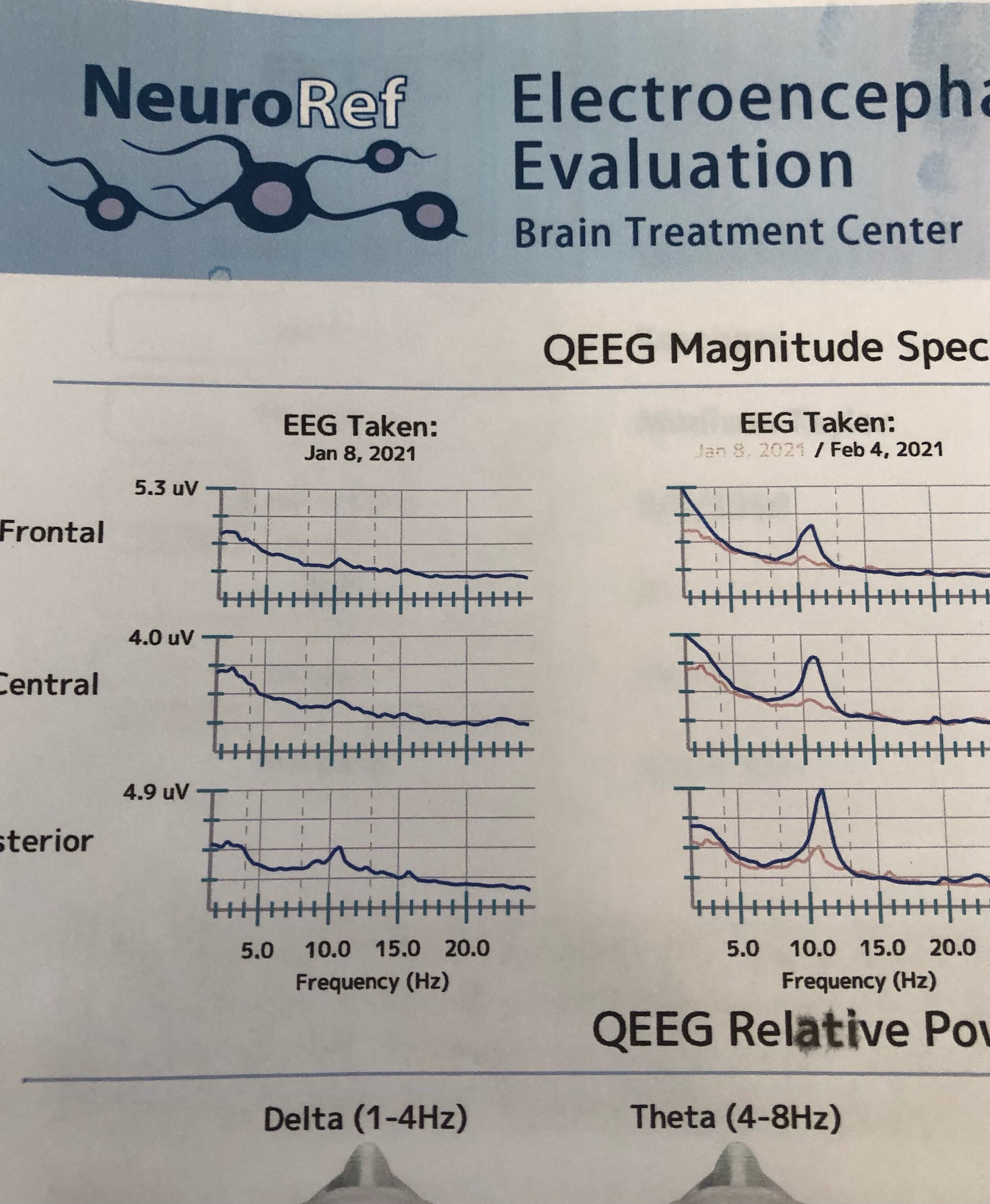
Changes in Madison’s EEG seen after a month of treatments.
NCSA: Did Madison’s EEG change after the treatment?
JK: Yes her EEG did change. The brain waves increased. So there seems to be an objective measure of improvement and not just our anecdotal observations.
NCSA: I wonder if the benefits you are seeing will be lasting.
JK: We don’t know. We shall see.
NCSA: Jan, thanks so much for taking the time to share your experience with our NCSA community.
_______
For further reading:
Casanova MF, Shaban M, Ghazal M, El-Baz AS, Casanova EL, Sokhadze EM. Ringing decay of gamma oscillations and transcranial magnetic stimulation therapy in autism spectrum disorder. Applied Psychophysiology and Biofeedback. 2021 Jun;46(2):161-73.
Casanova MF, Shaban M, Ghazal M, El-Baz AS, Casanova EL, Opris I, Sokhadze EM. Effects of Transcranial Magnetic Stimulation Therapy on Evoked and Induced Gamma Oscillations in Children with Autism Spectrum Disorder. Brain Sciences. 2020 Jul;10(7):423.
Casanova MF, Sokhadze E, Opris I, Wang Y, Li X. Autism spectrum disorders: linking neuropathological findings to treatment with transcranial magnetic stimulation. Acta Paediatrica. 2015 Apr;104(4):346-55.
Robison, John. Blogpost: TMS and Autism. http://jerobison.blogspot.com/p/use-of-tms-transcranial-magnetic.html
Disclaimer: Blogposts on the NCSA blog represent the opinions of the individual authors and not necessarily the views or positions of the NCSA or its board of directors.