Jackie with Vanessa Rastovic, Achieva DHI Policy Manager
NCSA joined IDD healthcare leaders in Chicago last week to challenge the status quo of antiquated, siloed health systems – calling for a reimagining of specialized integrated multidisciplinary healthcare. NCSA Policy Director Jackie Kancir attended the One Voice Conference hosted by the American Academy of Developmental Medicine & Dentistry (AADMD).
Respite — What’s That?
A few months ago, Steve Perlman, DDS, one of the founding members of AADMD, urged me to attend their conference in Chicago. I felt honored for the invite, but I am a full-time caregiver to a daughter requiring high acuity care living in a state with nothing that resembles what she needs. I’m on duty all the time. The only “respite” I have had in the past five years has been for brain surgery and follow-up surgeries, and even then, my mother had to fly-in and take unpaid time off.
I told Steve there’d be no way I could leave for a weekend. If ever I was to find a way to acquire respite, I can’t say going to sit in a room with talking about issues I live out every day would be on the top of my list. Steve was insistent, though, and he continued to reach out to see how he could help with any of my efforts.
In the weeks that followed, Steve put his words into action – he was determined to help make a difference. I had mentioned a concern about negative outcomes I was seeing, despite highly treatable conditions such as UTIs, in emergency departments for people with profound autism and related disorders. Before I knew it, he had an email thread going with physicians from across the nation brainstorming viable solutions. Next, he sent me an article for review by physicians to publish on the topic. Steve was proving to me these weren’t typical “talkers.” These were the doers.
A fellow parent of an adult with SynGAP1-RD, recognizing the importance of my attendance, graciously offered to keep my daughter, and off I went. (Thank you, Heather, for the skill and love you poured into Jadyne. I was overcome with gratitude for your kindness.) Though my daughter has an empty waiver, one that says on paper I should get respite but can never provide it, a separate community program came to the rescue. The Tennessee Respite Coalition provided a grant that enabled me to attend the conference. If you live in Tennessee, I highly recommend reaching out to them. They make the process very simple.
The AADMD conference brings clinical, educational, and public health policy experts together to discuss practical solutions aimed at resolving healthcare disparities for people with intellectual and developmental disabilities.
The five-star bowl of alphabet soup included speakers from the Association of American Medical Colleges (AAMC), American Dental Association (ADA), Centers for Disease Control and Prevention (CDC), the President's Committee for People with Intellectual Disabilities (PCPID), and many others.
Caregiver Burden
Families often express their disdain for the siloed ineffective healthcare systems that fail to adequately serve people with intellectual disability, profound autism, and related disorders. These physicians were echoing the same disdain – from within the system – and turning ideas for solutions into reality.
I have written my fair share of one-pagers over the years, and while cleaning up files last week, I came across one from 2019 that I wrote to advocate for the Ending the Diagnostic Odyssey Act.
“Time spent this year transporting and attending appointments: 21,000 minutes (350 hours or 2 weeks)”
“Number of Specialists: 24 Current (over 100 lifetime)”
“Number of Hospital Admissions: >30” … .
When most people hear “caregiver burden,” I think they assume parents are complaining they missed a nail appointment. Caregiver burden for families caring for a loved one with severe or profound forms of autism is, in reality, something even the most articulate writers would find onerous to accurately convey to someone who hasn’t lived it. I’m no Jane Austen, so I won’t even try. For those that do get it, allow me to provide you some hope that this group that met at the AADMD Conference, they get it, too, and they want to fix that.
Hope Renewed
While appearing on a recent podcast, I was asked, “What do you do for fun?” Besides the question catching me off guard (24/7/365 caregiver, remember?), I answered, “This. Changing the whole damn system. That’s what brings me joy.” Although my party-type fun muscles have likely atrophied long ago, truly nothing would make me happier than leaving my daughter a world that has a system of supports that actually works for her so she can enjoy life to its fullest.
In that regard, being around these motivated disruptive healthcare leaders in Chicago was some of the most fun I’ve had in a very long time. It was like taking that first breath of fresh pine-soaked air in Yellowstone after choking on city smog for years. One breakout to another, I heard authentic understanding of the unmet needs of this population, reasoned and innovative solutions, and collaborations among a variety of disciplines.
Jackie Kancir, NCSA Policy Director (center) with Allen Wong, AADMD Immediate Past President, and Dian Chin Kit-Wells, AADMD President-Elect
The transformational leadership presentations brought me to tears. I was immeasurably grateful to these heroes who should all have been retiring in the Maldives by now but instead had chosen to dedicate their lives to this population, even knowing that meant clinics with 80% Medicaid patients, patients who would take 3-4 times longer to treat, and reimbursement rates that did not come close to the PPO rates they could have received had they chosen to serve any population other than ours. Barriers to care aren’t just on our end. Physicians face barriers to providing care for our population. They’re looking to change that, too, and I’m eager to assist.
Jackie and Steve Perlman, DDS, Co-Founder AADMD, Special Olympics International Liaison
Key Topics
Integrated Healthcare
What if instead of hundreds of hours spent in and driving to dozens of specialty appointments each year, your loved one’s care was all under one roof? What if the specialists didn’t just stack appointments but actually co-treated and worked in concert together? What if the physicians actually all communicated with one another with a transdisciplinary approach? The future is here with specialty clinics like Kramer Davis Health.
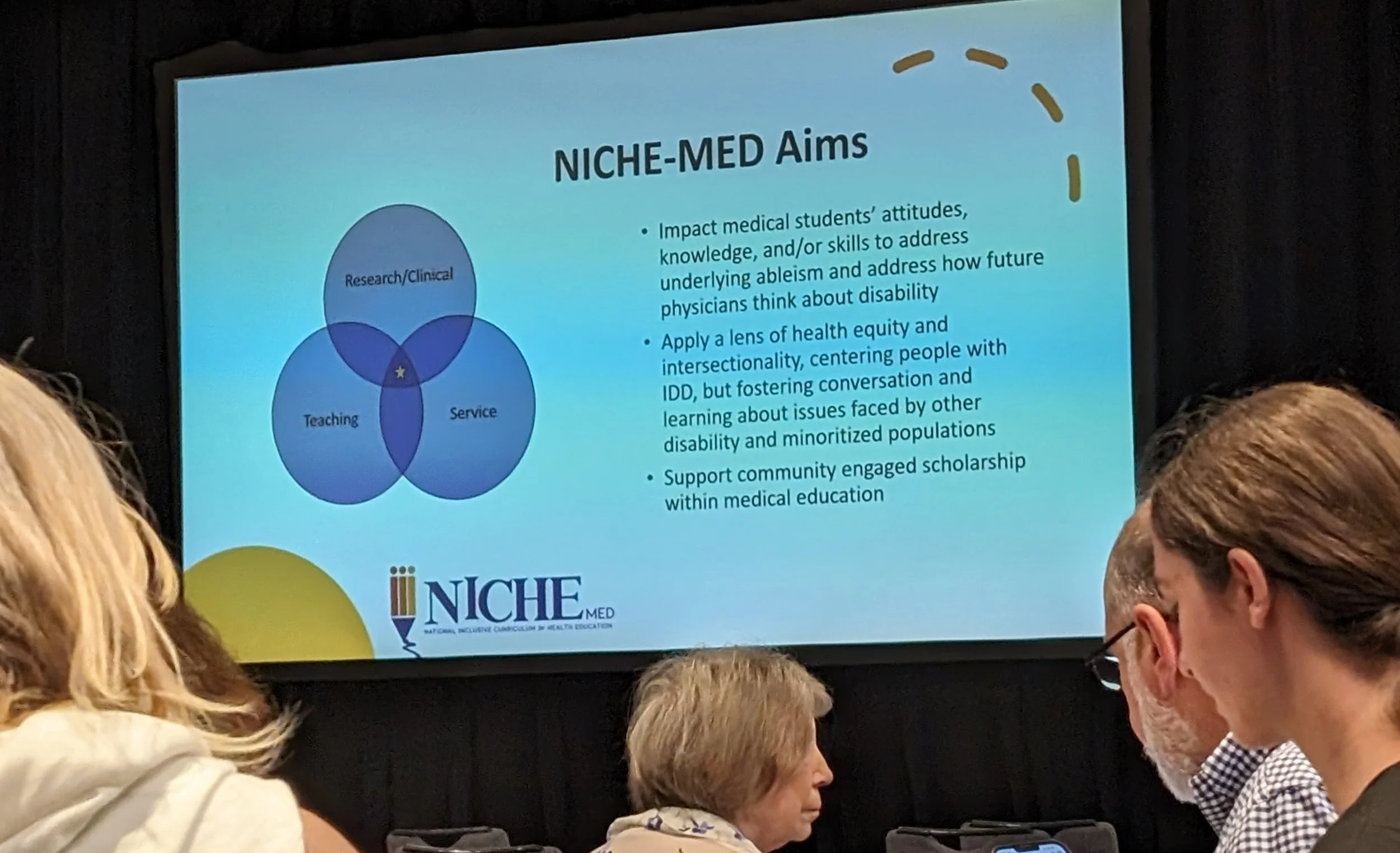
Improving Medical Education
What if more doctors knew about the specialty treatment our community needs? What if they received a specialized curriculum before even graduating? That is exactly what the NICHE program has already made happen.
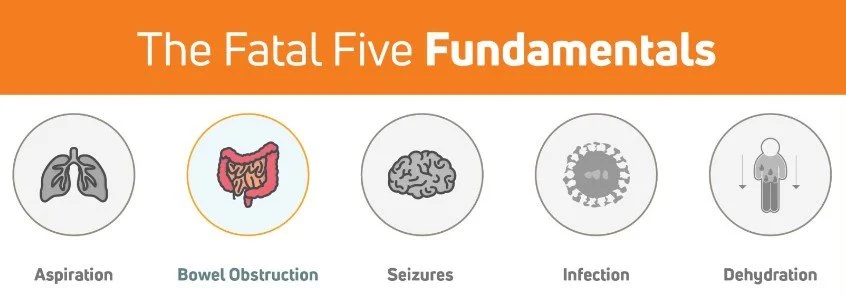
Reducing Risk
What if there was a tool to help identify preventable health risks and train anyone caring for an individual what to do to improve health outcomes and improve person-centered support? That is what IntellectAbility is all about!
BioPsychoSocial Models
What if ABA providers acted as patient advocates and partners with physicians? What if they used their data to help treating physicians narrow down options to explore for underlying medical conditions instead of rigidly insisting every behavior can be modified through a remedy for one of four functions? This new approach of an Intensive Behavior Interventionist was displayed by Crescent Behavioral Health. They even talked about their mobile behavioral health clinics, reducing the strain on patients by treating them in their own comfortable environments!
Ley Linder, Intensive Behavior Interventionist
Conclusion
The food was great, the company even better, and the content left a lasting impression that renewed my hope in better tomorrows for our children. In the coming months, NCSA hopes to provide you with webinars and podcast content by several of these inspirational leaders so you can hear for yourself what an incredible difference they’re making.
Until then, keep standing for what’s right. Keep defending reality. Though the healthcare system currently is incredibly tiresome to navigate, teams are working hard to develop innovative solutions. Together, we can end discrimination of severe and profound autism, break down antiquated silos, and build integrated healthcare that provides meaningful holistic specialized care. The future looks bright.