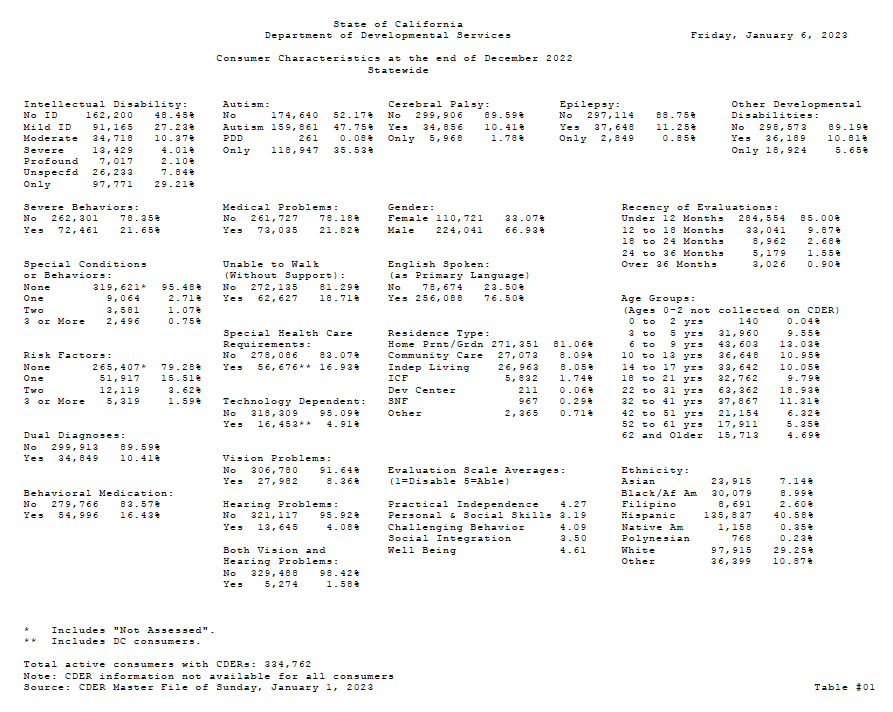
Autism caseload in California’s Department of Developmental Services continue to soar, as of the end-of-2022 count.
Read moreCDC: Autism Rates in U.S. Children Continue to Rise — to 2.76%, or 1 in 36
Over 20 years of ADDM surveillance the autism rate has climbed dramatically, more than 4-fold: now 1 in 36, for children born in 2012, compared to 1 in 150 for those born in 1992. Put another way, from .67% to 2.76%.
Read moreLancet Report: Momentum builds toward breaking up the autism spectrum
Dear NCSA community,
In October, NCSA published its position statement calling for categorical recognition of severe autism in the DSM. We emphasized the irrationality of an ASD diagnostic label that includes both "a young man with no language, a low IQ, few functional abilities, and aggressive, dangerous behaviors" as well as "a college professor with social anxieties and some OCD."
This galactic overbreadth subverts the essential purpose of psychiatric diagnostic labels: to describe a group of patients afflicted by a consistent set of impairments for the ultimate purpose of guiding meaningful interventions, services, and research.
We are hardly the only voices decrying the DSM-5's nonsensical scheme. And today a prestigious commission from The Lancet endorsed the use of the term “profound autism” to distinguish and support individuals who have high dependency needs and are likely to need 24-hour care throughout their lives.
Below are commentaries on this direction from NCSA board members Alison Singer, Amy Lutz and Jill Escher.
We are excited to see a larger movement toward a diagnostic scheme that reflects the realities and needs of this population, which includes some of the most devastatingly disabled patients in the entire field of psychiatry — and who must no longer be hidden in a category increasingly associated with "differences" and "strengths."
—NCSA
Labels can harm, but they also can help: See ‘profound autism’
From Stat News
A Lancet Commission report sets out priorities for autism research and practice, including a new designation for “profound autism.”
By Alison Singer
Labels are a divisive subject. When used inappropriately, they have the power to misrepresent and dehumanize people. As the mother of a child with autism, I have seen numerous instances in which hurtful or inaccurate labels have been applied to my daughter. Yet there are times when using accurate labels can dramatically improve the lives of those with autism. The specific label I’m thinking of is “profound autism” — and it’s one being embraced by an increasing number of autism researchers and advocates.
On Monday, The Lancet published a special report by The Lancet Commission on the Future of Care and Clinical Research in Autism, of which I am a member. In the report, several colleagues and I introduce the term profound autism to highlight the needs of people who cannot speak for themselves.
The term profound autism is intended to describe autistic people who are likely to need 24-hour support throughout their lives. The goal of introducing this designation is to provide more specificity to the extremely broad autism spectrum to equip parents, service providers, and the public with the language necessary to ensure that individuals with autism receive the accommodations and interventions they need. Concise, meaningful terms like profound autism will simplify the process of determining appropriate care, leading to quicker and more forceful interventions....
This muddle has had catastrophic consequences for those who, like my son Jonah, fall under the category of profound autism. Not only has their exclusion from research been well-documented, but their policy needs and preferences have been eclipsed by those of high-functioning autistic self-advocates who have spearheaded the ongoing fight to close the intensive, disability-specific settings that are often most appropriate for those who struggle with aggression, self-injury, and elopement. As the Commission noted, the most affected population is "at risk of being marginalized by a focus on more able individuals."... Read more
Lancet Commission Calls for New Category: "Profound Autism"
Pressure mounts to split the broad autism diagnosis created by the DSM-5.
By Amy Lutz, in Psychology Today
Yesterday, the Lancet Commission on the future of care and clinical research on autism — a group of 32 researchers, clinicians, family members, and self-advocates from around the world — released a comprehensive 64-page report detailing changes that should be made over the next five years to improve the quality of life of autistic people and their families.
Besides a common-sense call for individualized, incrementalized, evidence-based interventions, one of the Commission’s key recommendations is to carve out the most impaired section of the spectrum and give it its own label of “profound autism,” which would include autistic individuals who also have significant intellectual disability (IQ below 50), minimal or no language, and who require round-the-clock supervision and assistance with activities of daily living. The Commission expresses “hope that [the introduction of “profound autism”] will spur both the clinical and research global communities to prioritise the needs of this vulnerable and underserved group of autistic individuals.”... Read more
Podcast interview calls out absurdity of over-broad autism spectrum
Thanks to Mary Barbera for hosting NCSA President Jill Escher on her latest podcast episode. In addition to the failings of autism diagnostics they discuss new directions for autism research, exponentially increasing autism rates, NCSA, and national autism policy (or lack thereof). Listen in
Have an opinion about breaking up the autism spectrum? Join the conversation on NCSA's very active Facebook page.
See NCSA's position statement on the need for categorical recognition of severe autism in the DSM.
NCSA Calls for Categorical Recognition of Severe Autism in the DSM
Virtually all of the problems that recur … stem from, or are worsened by, the lack of a unique diagnosis for severe autism and the devastating symptoms that often accompany it.
Read moreSevere Autism: Stuck in the “Circle of Strife”
An autism mom calls for an integrated care approach for the severely autistic.
Read moreThe Sia Shaming Spectacle Is a Tragedy for the Arts and the Autism Community
Publicity shot from the new film “Music,” by the Australian artist Sia.
By Jill Escher
Humans have a long tradition of public shaming spectacles. Think of the public hanging of criminals, the burning of heretics at the stake, the guillotine-ing of aristocrats, the stoning of women accused of adultery.
But in our modern era the spectacles are more likely to take place online by outraged (or, more likely, mildly ruffled and anonymous) mobs who gleefully dogpile on hapless victims after the latest e-fatwa is announced by their leaders.
It only takes about 30 seconds of your time, provides a rush of sanctimonious satisfaction, and, best of all, it’s free! Can you say, “Cheap Thrills”?
Yes, the singer/filmmaker Sia is the latest casualty to succumb after committing a truly TERRIBLE SIN … an unforgiveable transgression of the Book of Neurodiversity … she cast an actor in the role of a girl with severe autism in her new film “Music” … and that actor was only pretending to be that character! OMG, shut the door! Daniel Day Lewis you are cancelled! Eddie Redmayne you too are cancelled! Dustin Hoffman, consider yourself cancelled! Every actor who has ever played someone beset by a condition they didn’t actually have, enjoy the gruel in Cancel Jail! (Goodbye Leonardo DiCaprio, and oh no, also Russell Crowe, I am sobbing….)
The attack on Sia by a vocal, unhinged minority is so preposterous that one would normally shrug it off with a “Oh, there go those-people-who-have-so-much-time-on-their-hands-they-attack-a-stupid-puzzle-piece,” but in reality this is much worse. This time, evil has triumphed.
Evil because the crusade to crucify Sia sends a diabolical message to every person in the performing arts: depict severe autism in your movie/film/play at your own peril. If you don’t do it exactly the way we want, you are toast. Transgress the Book of Neurodiversity in even the slightest manner and you will be pilloried, putting at risk months and years of creative effort and financial investment. Your reputation will be stained. Your artistic freedom squashed.
In other words, what artist would dare to tread on the subject matter of severe autism when a tidal wave of mindless insta-denunciation awaits them, at the merest stroke of a self-righteous Tweet?
For that’s what’s at stake here — banishment of depictions of severe autism. As the autistic writer Lucy Kross Wallace observed:
“It is one thing to suggest that casting actors with disabilities might produce more compelling performances, but it is quite another to foist these requirements upon every artist. In calling for Music’s cancellation, neurodiversity advocates cross the boundary from exercising their own liberty to infringing on that of others, including Sia’s autistic collaborators.”
What a tragedy for the autism community. Children with severe forms of autism have become a vast proportion of the population, about 1 to 1.5% of all children! Clearly they deserve more and more representation — in the news, on film, on TV, on stage, in print, everywhere. But the hair-trigger threat of Neuro-scorn will surely help keep severe autism firmly in its dark corner, orphaned, abandoned from the broader autism discourse, despite the monumental societal urgency.
As the mom of a nonverbal autistic teenage girl who seems, based on the trailer (I haven’t seen the film, it’s not yet out in the US, and I should add that for all I know I won’t like the film at all), very much like the lead character Music. How fabulous that a filmmaker chose to make a movie with a character like my darling Sophie, it’s happy dance time! People like Sophie are so dreadfully hidden from public view. So my feeling was, hurray for Sia for shining an oh-so-rare light!
But — according to the mob but also Autism Speaks, which tweeted in support of the mob — no happy dancing for me, because someone like my dear Sophie was not cast in the lead role.
Okaaaaaayyyy… say what? Let me tell you what would have happened if Sia had cast Sophie as Music. She would have wandered off the set, flung off her costume and headphones, flipped out at the lights and noise, fell asleep at the late hours, and failed at following a single directorial direction. In other words, disaster.
This point was conceded by the mob, which instead took the position that Sia should have cast a girl with high-functioning autism who had the cognitive-functional capacity to perform in the role. Sure, okay, I saw the lovely film “Keep the Change,” which, for example, cast actors with high-functioning autism in the lead roles, and to my mind it was triumphant.
But, really, we can acknowledge that actors with autism or other disabilities can do great work and should be among those considered for roles of all kinds without the disproportionate hysterics of demanding that every single autism character be played only by those who pass some sort of bizarre spectrum purity test? Or should a zealous mini-mob wield veto power because through some loony logic that I have been unable to fathom, they own the whole turf of “autism”?
Yesterday I am told Sia took down her Twitter account after enduring months of attacks. I am told she apologized to the mob (for what, I’m not sure).
We are all losers here. The autism community. Artists. Writers. Actors. The public. Creative expression. Free speech. Disability awareness. And of course Sia herself.
It cost exactly nothing for vindictive and self-absorbed Sia shamers to cast a dark shadow on her heartfelt endeavor over a mere triviality. This is not how reasonable people behave. Reasonable people may write a negative film review (have at it!) but they don’t launch a cancel crusade over something as innocuous as casting choices (right, Daniel, Eddie, Dustin, Leonardo, and Russell? or shall we demand your penance too?).
The frightening bottom line here, to borrow the words of a neurodiversity leader, is that Bullying Works.
Jill Escher is President of the National Council on Severe Autism.
Disclaimer: Blogposts on the NCSA blog represent the opinions of the individual authors and not necessarily the views or positions of the NCSA or its board of directors.
California's Autism Explosion: An Eyewitness Perspective
“In the 1960s clinicians seldom encountered these sorts of very striking abnormalities, whatever the category name."
California Department of Developmental Services
Autism Cases by Birth Year
Autism cases by birth year, showing the growth in California Department of Developmental Services autism, from 0.001% in birth year 1931 to 1.18% in birth year 2012. Data from 2017. Graph from Nevison et al 2018.
The author
By Sue Swezey
A new paper looking at autism prevalence in California tells us what we old-timers already know: autism rates here have increased almost exponentially over the past several decades.(1)
Yet to this day, some academics suggest that the autism increase doesn’t exist.(2) These doubters question the consistency of data collection and point to greater skill on the part of diagnosticians, as well as to broadening of diagnostic criteria. A few even blame the victim, implying that grasping parents may seek the ASD label to obtain trendy services for their more typically functioning offspring, or that professionals may profit by jumping on the autism bandwagon. Who ever dreamed autism would have such cachet?
Doubters of the increase seem to accuse believers of some form of delusion, maintaining either that (a) there are really fewer children on the spectrum than people claim, and we are over-labeling milder disorders, or (b) there have always been huge numbers of children on the spectrum who went all but unnoticed until recently. Pick your fallacy.
While Nero fiddles and academics bicker, one thing is beyond dispute: agencies are increasingly hard-pressed to meet the immense needs of the rapidly growing caseloads of disabled young adults, and special ed classes overflow with ASD children, where just a few decades ago only a handful were seen. Families are growing desperate for lifespan services, and housing demand massively exceeds supply.
As the parent of a 55-year-old son with autism (who still lives at home, with me), and as someone who has been an active autism advocate for nearly five decades, I am puzzled. If there has really been no increase over the last 55 years, then there must have been an equally large percentage of children on the spectrum when John was little. How could it be that I never encountered them? As a youngster, John was memorable in any setting. Were all the others so well behaved, so very mildly disabled, that no one noticed?
“If there has really been no increase over the last 55 years, then there must have been an equally large percentage of children on the spectrum when John was little. How could it be that I never encountered them?”
The author’s son as a toddler
Back in the 1960s, there were only a handful of other children in our entire county with impairments like his. John was born in 1963, likely part of an autism blip resulting from an outbreak of German measles.(3) When he was finally diagnosed at age six, conventional wisdom counted 4:10,000 (1:2,500) with the autism label,(4) a far cry from the 1:59 which the CDC cites today.(5) What accounts for the immense discrepancy between then and now?
“His pediatrician had seen only one other case like John’s in 20 years of practice.”
All I know for sure is that John’s history is that of a little boy very much alone with his diagnosis. His San Mateo pediatrician had seen only one other case like John’s in 20 years of practice. It took six years and a succession of experts to award him with the autism label, with stops along the way for learning disabled, neurologically handicapped, emotionally disturbed, childhood schizophrenic, and “troubled” (this from a therapist who didn’t like labels, so invented his own). While John would now be considered classically autistic from an early age, his symptoms under any label were then extremely rare. We can certainly agree that diagnosis has improved since his childhood, but that cannot explain that in the 1960s clinicians seldom encountered these sorts of very striking abnormalities, whatever the category name.
In the community, no one knew what to make of John, or of his suspected “Refrigerator Mother,” as we were sometimes called. They had never seen anyone like him before. As a rapidly regressing preschooler, he desperately needed help. While no one knew what to do, everyone seemed to have firm opinions. A school psychologist blamed John’s total lack of social skills on Sunday school avoidance (though I fear even Jesus might have been hard pressed…). Well-meaning neighbors insisted that the neighborhood co-op would bring miracles of socialization; the actual result was to make him one of the earliest and most miserable victims of forced inclusion. (As parents know, inclusion can be wonderful when it's done right. This wasn’t.)
In the late 1960’s John was registered with the San Mateo school district, as required by law – not that he could attend, because public schools did not then have a legal mandate to serve children with autism. At the time, the San Mateo district was aware of only one other child with autism, as was also the case when we moved down the county to Menlo Park in 1973. (Note: San Mateo County now has about 1,000 cases of autism in the state Developmental Services system, comprising about one-fourth of the total developmental disability caseload in the county.)
Programs specifically designed for autism did not exist at the time of John’s diagnosis. The scattered children with autism were so few and far between that they had to squeeze into programs for other disabilities, or for the emotionally disturbed. Often the few children who did not fit into public school were farmed out to programs outside their districts, sometimes far from home or even out of state.
California DDS autism prevalence among 8 year-olds (purple), compared to 8 year-olds from the IDEA and ADDM networks. DDS prevalence, while still clearly growing since the 1980s, may be lower because it includes only the more severe (developmental disability level) cases. Graph from Nevison et al 2018.
In fact, the first Autism Society of America (ASA) chapter in San Mateo County could find so few members that we met jointly with parents of adult schizophrenics. We called ourselves PASCA, Parents of Adults with Schizophrenia and Children with Autism. We had little in common except that our scant funding came through Mental Health, though we did share the bond of being rare outcasts in neighborhoods full of “normal” families. At the time, some autism professionals considered those rare cases of autism to be a form of childhood schizophrenia, with meager research being reported in the Journal of Autism and Childhood Schizophrenia.
In the early days of our ASA chapter, we were desperate to get our children into the Regional Center system, where they could be treated as developmentally disabled rather than disturbed and could gain access to appropriate programs and services. Here again we were hampered by our small population. We early advocates besieging Sacramento tried to give legislators the impression that we were a much larger group and sometimes resorted to disguises, complete with wigs and quick wardrobe changes.
By the late 1970s autism was finally included in the Regional Center system. Even with its case-finding mandate, autism barely registered in the overall caseload. It was not until the late 1980s that we became aware of a significant autism increase. At that time California’s DDS saw an inexplicable surge in cases, prompting them in the late 1990s to review their growing caseloads for an explanation such as diagnostic shift (their review could not locate any sociological or diagnostic explanation for the increase). The Autism Research Institute also noted the start of a surprising rise in incidence.
Lurking in the background all this time was the DSM (Diagnostic and Statistical Manual of Mental Disorders). Revisions over the years have encompassed changing and often controversial views of autism, which some blame for the apparent increase in autism’s prevalence. But reports here in California of exploding prevalence have come mainly from agencies evaluating children under developmental disability criteria that have grown more stringent over time, not more generous. While the DSM can reshape the elusive boundaries of autism, in California our hard-core DD-level autism has grown from fewer than 2,000 when John was a boy to more than 108,000 today. DSM’s fluctuating definitions have prompted a lot of quibbling, but perhaps the most compelling evidence for an autism increase comes from the desperate need for services from the unquestionably expanding population of young adults too mentally disabled to care for themselves.
Has increased awareness created the illusion of an autism surge? I simply cannot imagine that there were tens of thousands of children with autism who were undiagnosed or misdiagnosed over decades. If such a huge population had existed, they surely would have been conspicuous enough to attract attention, at least if they were anything at all like John. Physicians encountered so few patients with autism traits that our ASA chapter actively tried to promote physician awareness by papering doctors’ offices with homemade flyers entitled, “Your Next Patient Has Autism.”
Yes, in John’s lifetime diagnosis has improved, diagnostic criteria have broadened, and diagnostic methodologies continue to evolve. But this progress cannot explain the supposed missing masses of children whom we somehow failed to detect under our noses half a century ago. If the incidence were really the same then as now, John's childhood must have been populated with phantom children whom we never saw. The clinicians never saw. The teachers never saw. The neighborhoods never saw. The Regional Centers never saw. The institutions never saw. There is no documentation anywhere to suggest the existence of these shadow children, except in the minds of some academics.
Sue Swezey is the mother of an adult son with autism. She co-founded the San Mateo County Autism Society, now part of Autism Society San Francisco Bay Area, and served on the Executive Committee of the San Mateo County Developmental Disabilities Council. She also served on the Morgan Autism Center board from 1974-2012. Sue was one of the first to report on uses of technology for special needs and published a special education technology journal from 1981-2009. She lives in Menlo Park, California, with her son John.
A version of this blogpost was first published on the blog of Autism Society San Francisco Bay Area in September 2018.
References:
(1) Nevison C. et al. California Autism Prevalence Trends from 1931 to 2014 and Comparison to National ASD Data from IDEA and ADDM. J Autism Dev Disord. 2018. July 5.
(2) See, for example, Fombonne, E. The rising prevalence of autism. J Child Psych. and Psychiatry 2018;59:7,717-720.
(3) See, for example, Chess S. Autism in children with congenital rubella, J Autism and Childhood Schizophrenia1971;1(1):33-47. Also discussed in the 1970’s in The Advocate, the newsletter of the National Society for Autistic Children (NSAC). NSAC was the predecessor of ASA but served only school-age children and their families, since there were few known adults with autism at the time.
(4) See, for example, Fombonne, E. Is there an epidemic of autism? Pediatrics 2001;107:411–412. Also reported by NSAC. Research was scarce at the time, since autism was not considered statistically significant enough to warrant funding.
(5) Baio J, et al. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. Surveillance Summaries / April 27, 2018 / 67(6);1–23. This surveillance study identified 1 in 59 children (1 in 37 boys and 1 in 151 girls) as having autism spectrum disorder.
Note: NCSA and the author wish to emphasize this from the NCSA FAQ: “[T]he vast majority of autism cases today are still considered ‘idiopathic,’ in other words, having no identified cause. There is no evidence linking the rising prevalence of autism to childhood vaccines, or vaccines given in any other developmental window. We encourage parents to ensure their children are fully vaccinated in accordance with the recommendations of the American Academy of Pediatrics. Infections resulting from failure to vaccinate can cause serious harm to a child, including brain damage and death.”